

Hookworm-related cutaneous larva migransis endemic in many resource-poor communities in the global South ( 19, 24, 28, 29, 35, 42, 43). The risk of infestation is up to 15 fold higher in the rainy season as compared to the dry season ( 29).
In warm-climate countries, there is a distinct seasonal variation of hookworm-related cutaneous larva migrans, with a peak incidence during the rainy season.

sandals on the way to the beach and on the beach - may reduce the risk of infection ( 50). In a study in rural Brazil young age, male sex, living in a house without a solid floor, always walking barefoot on the soil and the presence of animal faeces on the compound were identified as independent risk factors ( 28). Apparently, the material had been soiled by cat excreta when deposited in a humid shed. In Naples, Italy, a small epidemic occurred in customers who had bought dry flowers, bark and spikes to prepare floral arrangements ( 22). For instance, if washed clothes are dried on the ground, larvae may creep on the textile from surrounding soil, resulting in infection when the piece of clothing is worn. In Serbia, a man developed multiple lesions on his back after having repaired his car in a garage laying below a car and wearing only shorts ( 49).Įxceptionally, larvae may be transmitted through fomites. In Kuala Lumpur, a native visitor became infected when he took showers in a bathroom, soiled with cat excreta ( 40).
Treating hookworms in humans skin#
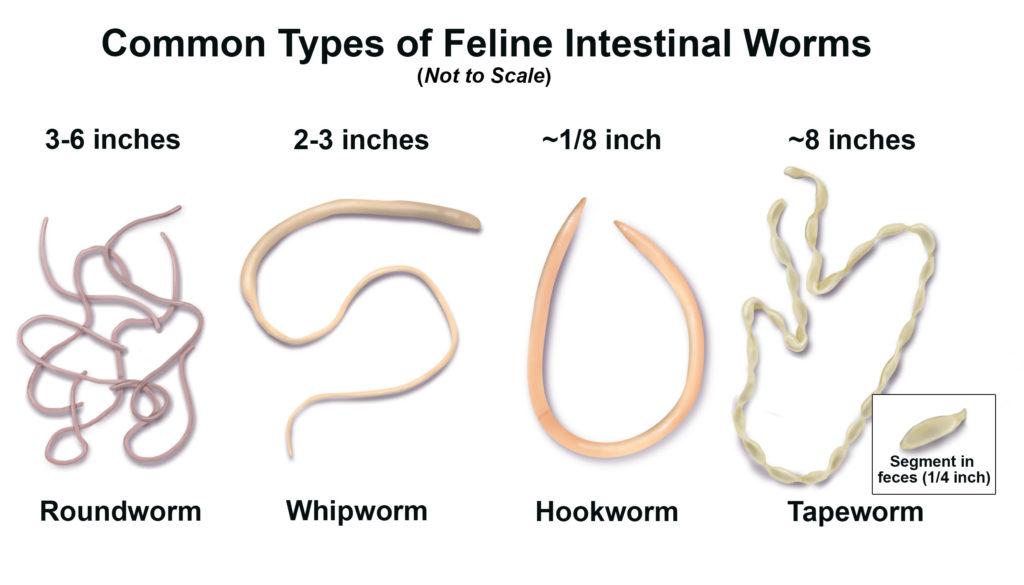
Depending on local clothing habits and age-specific behavior, other areas of the skin may be exposed ( 31). Walking barefoot is probably the most common type of exposure. Transmission occurs when naked skin comes into contact with contaminated soil. Other nematodes of domestic and wild animals may also causehookworm-related cutaneous larva migrans. Usually,hookworm-related cutaneous larva migransis caused by hookworm larvae from dogs and cats ( Ankylostoma caninum, A. How rapidly a larva can penetrate the stratum corneum of the epidermis remains unknown. After having located a host, larvae creep across the skin and probe sites suitable for penetration into the epidermis ( 25). Under favorable environmental conditions, larvae can survive and remain infectious for several months. They develop into infective third-stage larvae after about one week ( 2). Eggs are shed in faeces and hatch in the superficial layer of the soil within one day. Biology, Transmission and Risk FactorsĪdult hookworms live in the intestine of dogs and cats. In countries of the global South as well as in travelers returning from an endemic area, hookworm-related cutaneous larva migrans is the most common cause of a creeping eruption. This clinical sign can be provoked by different parasites, such as animal hookworm larvae, other nematode larvae, Gnathostoma spp, Loa loa, Sarcoptes scabiei(scabies mites), or larvae of parasitic flies (migratory myiasis). The latter is defined as a linear or serpiginous, slightly elevated, erythematous track that moves forward in the skin in an irregular pattern. ( 10) correctly pointed out that cutaneous larva migrans is a syndrome while creeping eruption is a clinical sign. For decades, the terms creeping eruption and cutaneous larva migrans have been used interchangeably. Hookworm-related cutaneous larva migrans (HrCLM) is a parasitic skin disease caused by the migration of animal hookworm larvae in the epidermis.


 0 kommentar(er)
0 kommentar(er)
